Pancreatitis Ayurvedic Treatment: Holistic Care for Pancreatitis
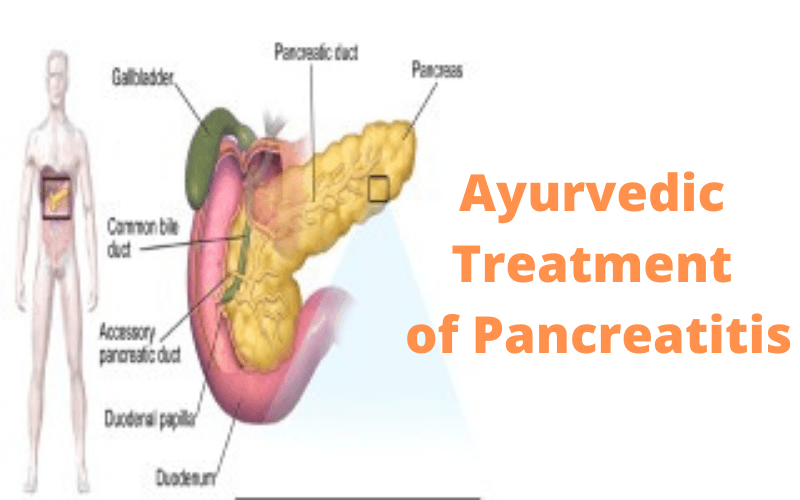
The inflammation of the pancreas is called Pancreatitis. The pancreas produces hormones and enzymes that assist in the digestive process, produces glucagon and insulin hormones that help regulate the way the body processes sugar (glucose).
The pancreatitis condition can occur as acute pancreatitis that appears suddenly and lasts for some days, or pancreatitis can occur as chronic pancreatitis, which occurs over many years.
The Ayurvedic treatment for acute and chronic Pancreatitis has worked wonders in improving the patients’ medical conditions over the years, as the gut-related disorders are best managed with the help of Ayurvedic treatment.
In Pancreatitis, pancreatic digestive enzymes are activated before they are released into the small intestine and begin attacking the pancreas, causing inflammation and showing pancreatitis signs and symptoms. With repeated bouts of acute pancreatitis, continuous damage to the pancreas occurs and leads to chronic Pancreatitis. A poorly functioning pancreas can cause digestion problems and diabetes.
The utility of Ayurvedic treatment for diabetes is well recognized now since all the knowledge given in ‘Samhitas’ holds even proper now, and modern science is just validating. The best example of this claim is revering diabetes mellitus completely in patients of ‘Sthol-Kaya‘ or over-weight.
Ayurvedic Treatment Of Pancreatitis
In Ayurveda, the pancreas is known as ‘Agnashaya’ or ‘Grahani‘ or the seat of Agni (body fire) in the body. Pancreatitis in the initial phase is an imbalance of Vata-Pitta, but later on, a ‘Pitta’ disorder that disturbs the function of ‘Agni‘ in the body.
It leads to aggravation in digestive fluids in the pancreas. It is at the time of acute condition when a patient should start seeking treatment for Pancreatitis.
The treatment focuses on curing the symptoms, thereby reducing the future chances of relapse. This is being done with the ancient three pillars approach of Ayurveda that focuses on Aahar(Diet), Vihar(Lifestyle), and Ausadh(Medicine).
This approach has been proven successful as doctors or dietitians seldom spend much time with their patients.
The treatment focuses on identifying their Prakriti to plan their treatment as what suits their gut and intends to gradually add the meals in their regimen, which ones they have been asked to stop forever.
Types of Pancreatitis
Acute Pancreatitis –
In acute Pancreatitis, there is a sudden inflammation of the pancreas with pain and raised levels of amylase and lipase in the blood and urine. It varies to have lesions, necrosis of the parenchymal tissue, pancreatitis fat necrosis.
Chronic Pancreatitis –
In the chronic stage, which happens due to long-standing changes, degenerative changes are observed, including the atrophy and calcification of the pancreas. There is a progressive loss of exocrine and endocrine functions of the pancreas.
Signs & Symptoms
- Acute upper abdominal pain radiating to the back worsened after meals.
- Poor control of blood sugar.
- Nausea and Vomiting, tenderness over abdomen.
- Recurrent and persistent abdominal pain.
- Weight loss without any workout or physical effort.
- Oily and smelly stools (Steatorrhea).
- Increase enzymes( Lipase and Amylase) levels in the blood/urine ( Pathological features).
- Gall stones/sludge, Pancreatic oedema, calcification of pancreas, pancreatic necrosis, pseudocysts and duct strictures ( Radiological findings)
Causes and Risk Factors
The exact cause or causes of Pancreatitis remain unknown, but some of the risk factors and causes that have been identified now are related to Pancreatitis.
1. Genetics:
Genetics have been shown to cause Pancreatitis with mutations in the genes as CFTR, SPINK1 and PRSS1.
2. Alcoholism:
Long-term alcohol users, i.e. chronic alcoholism, are related to the cases of Chronic Pancreatitis.
3. High calcium and triglycerides:
High calcium and high triglycerides levels in the blood are the conditions that can lead to Pancreatitis.
4. Medications:
Corticosteroids like prednisolone, HIV drugs as pentamidine, didanosine, diuretics, and anticonvulsants like valproic acid, the chemotherapeutic agents have been associated with the condition.
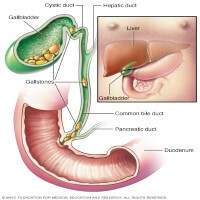
5. Gall-bladder stone:
Stones in the gall bladder are the most common cause of acute Pancreatitis. These gallstone/s block the pancreatic duct, trapping digestive juices inside the pancreas. Women older than 50 years are more likely to get pancreatitis due to gallstones.
6. Autoimmune:
This happens when the body’s autoimmune cells affect the healthy cells of the pancreas.
7. Infection:
Infection from viruses like mumps, varicella, herpes, bacterial, and fungi may be related to causing Pancreatitis.
Self Care Tips
- The Ayurvedic treatment of pancreatitis takes time and so one should keep patience while getting it treated. Self-control and lift the spirits are must to begin the treatment.
- Herbs that improve digestion and have anti-inflammatory properties need to find a place more on the dining table.
- Alcohol and tobacco should be avoided even in case of mild acute Pancreatitis.
- High-fat foods and heavy digestible items that clog the gut are not recommended to slow the digestive fire.
- The treatment requires self-control and pursuing a regimen that helps better function the gut with an improved ‘Agni’ to allow a person to eat meals that are usually restricted in the initial days of diagnosis of Pancreatitis.
- Maintaining the water intake during the day as per the body’s need is imperative as consuming less or more water can directly impact the digestion of the meals. Medicated buttermilk should be the drink of choice and to be taken in afternoon meals.
- Avoid foods that aggravate Pitta in the body.
Aas Ayurveda has the speciality in treating Pancreatitis. The focus of the treatment lies in restoring its normal functioning and prevent future relapse or deterioration of the condition. The management varies from one individual to another depending on age, body constitution, and how far the disease has progressed. The health seekers who started treatment of Pancreatitis with us have their hba1c levels within the normal limits, curtail or stopped their medicines for diabetes completely. Once the patients complete their treatment protocol, the medications are removed from their treatment journey.